Diabetes: A Mahorize woman experiments with a new model of artificial pancreas
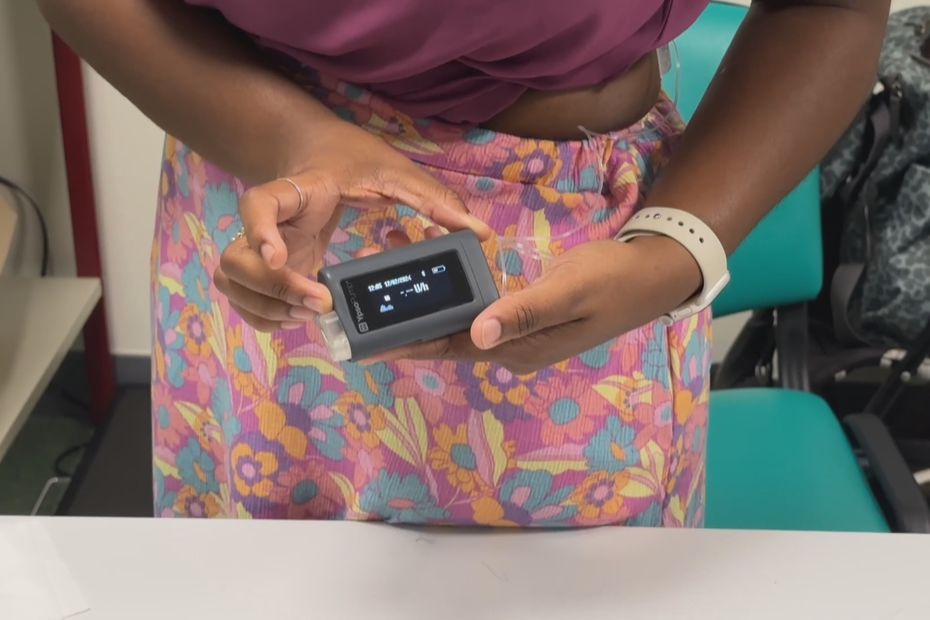
Since late January, Myla Manroff has been testing a new artificial pancreas model with Felix Guion University Hospital. A system that combines insulin pumps, blood glucose sensors and smartphones opens up new horizons for type 1 diabetics.
•
in the meeting, 80,000 people have diabetes. 10% of them are affected by type 1 due to lack of insulin secretion by the pancreas. The purpose of the device is to better control glycemic peaks, which avoids daily fatigue, and in the long term, complications of the disease.
See the report from Reunion La 1re:
Diagnosed with type 1 diabetes at age 11, Myla Manoff isn’t her first artificial pancreas. But the first device was “ Very restrictive » In the management of glycemic peaks. This new model, which Mahoraise has been testing for three weeks, has a more precise level of adjustment. Since then, the mother has seen a clear improvement in her quality of life, reduced hypoglycemia, reduced stress, with the only limitation of having another mobile phone with you at all times. Stabilization of sugar levels helps improve daily quality of life, eliminates fatigue associated with hypoglycemia, And avoid long-term complications of diabetes on the eyes, kidneys and heart.
For insulin-dependent people, at least 4 injections per day must be used. With this artificial pancreas, observational dosing allows administration and is limited to one injection every three days. Handling became easier for double-hatted Myla Manroff, both patient and nurse at CHM in Mayotte. However, the allocation of an artificial pancreas is accessible to most patients with type 1 diabetes. The device, connected to a smartphone, creates a link with nursing staff and alerts when hypoglycemia occurs. In case of repeated warnings,“The healthcare professional can approach the family to find a solution and possibly adjust the setting” Diabetologist Anna Floss of the CHU Félix Guyon explains.
Contributing to the Therapeutic Education Tool, diabetologist Anna Floss helps us measure the evolution of care over decades. In the 1960s, diabetes was still a deadly disease, fatal to sufferers. “in a few months”. Subsequently, the mortality rate decreased but patients were still promised Complications, such as visual impairment, amputation or heart attack. Today’s technology prevents the occurrence of these complications and improves the quality of daily life, so that the patient ” General professional and social activities.”